One of the primary responsibilities of healthcare entities is to ensure providers enlisted to render services through that entity are who they say they are - possessing the required training, skills and licenses needed to perform function successfully.
There are many moving parts to confirm these critical requisites - collectively referred to as credentialing. Delegating credentialing can be an effective solution for this labor-intensive and time-consuming operational requirement.
Below is a breakdown of all you need to know about delegated credentialing and other information you need to decide the best course of action for your organization
What is Delegated Credentialing?
Delegating credentialing is an arrangement in which a healthcare entity authorizes another healthcare entity to credential its healthcare providers - such as when a preferred provider organization delegates the provider credentialing process to a hospital. Beyond credentialing verification, the delegated entity is responsible for reviewing providers' qualifications and executing credentialing decisions on behalf of the delegating entity.
The spectrum of specific data required to make credentialing decisions can include:
- State licensure
- DEA Registration
- CDS (Controlled Dangerous Substance) Certification
- Board Certification/Specialty Information
- Education
- Malpractice History
- Professional Liability Claims Settlement History
- Work History
- Hospital/Facility Affiliations
- Disclosure Questions
- Attestation
- Sanctions & Exclusions
You can find more details on delegated credentialing in our handbook.
Ongoing Credentialing Obligations
Verifying data across the above spectrum can be burdensome even just once – but providers must be re-credentialed at least every two or three years at each facility and with each payer. This may include separate credentialing at each facility within the same organization.
Sounds like a lot (it is). The good news? The provider credentialing process is one your healthcare organization can outsource to another company. The two primary options for delegated credentialing include:
- Outsource to an external credentials verification organization (CVO). CVOs are specialized groups whose primary line of business is to perform primary source verifications for healthcare organizations.
- Establish an internal CVO. Healthcare organizations can establish a central office dedicated to performing primary source verifications for all health providers across all facilities.
Understanding Regulators and Delegating Credentialing
There are several regulators involved with or have an interest in delegated credentialing:
- NCQA (National Committee for Quality Assurance): NCQA’s mission is to drive improvement across the healthcare delivery system. NCQA guidelines are considered the gold standard for quality. In many cases, these guidelines form the basis of delegated contracts - meaning it is crucial for entities to review their standards and requirements thoroughly.
- CMS (Centers for Medicare and Medicare Services): CMS, an arm of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children’s Health Insurance Program (CHIP) and portions of the Affordable Care Act (ACA). Entities offering health services covered by these Federal health programs and looking to delegate the credentialing process should know CMS has additional requirements that go beyond the NCQA’s guidelines.
- Local state governments: Some local governments have other requirements for the credentialing process - including mandatory application, use of a universal organization to conduct primary source verification and/or specific turnaround times for credentialing processes.
Delegated Credentialing: An Increasingly Important Strategy
Demand for healthcare services is growing fast, and delegated credentialing can pay significant dividends in both time and money for healthcare organizations looking to keep pace with industry growth. Delegated credentialing can help reduce operational costs and support provider groups in having control and consistency in their revenue cycles.
Benefits of Delegated Credentialing
There are four strategic benefits associated with leveraging an internal or external CVO to manage and centralize the provider credentialing process:
- Reduced Payer Enrollment Timelines. Delegated credentialing agreements can greatly reduce the time it takes to successfully enroll a provider with a Health Plan. Without delegated credentialing, it can payers up to 120-160 days to credential a provider. Obtaining delegated credentialing agreements with payers can reduce this timeframe to 30-45 days.
- Medical Staff Bandwidth. Providers performing health procedures at several facilities within an organization carry an additional credentialing burden - each facility must verify the same credentials. Centralizing the process can help optimize the process and give the medical staff more time to attend to other responsibilities - including privileging and board approvals.
- Provider Time. In a normal scenario, providers working across separate facilities would need to individually complete credential verification paperwork for each facility. Centralizing the process saves providers a lot of time and reduces energy expenditure redundancies.
- Revenue. Reducing the overall amount of paperwork providers are responsible for frees them up to see more patients. Increased patient encounter volume directly correlates with organizational revenue and, ultimately, reimbursements.
- Patient Satisfaction. The initial credentialing process can take a great deal of time. Centralizing operations through delegated credentialing helps support faster onboarding for providers, reducing scheduling time and increases patient satisfaction.
How Verifiable Can Help
Leveraging the right partnership for delegated credentialing can help simplify your organizations’ day-to-day operational processes and promote much smoother operations for all involved - employees, the facility and the patients in your care. This translates directly into valuable time and money savings.
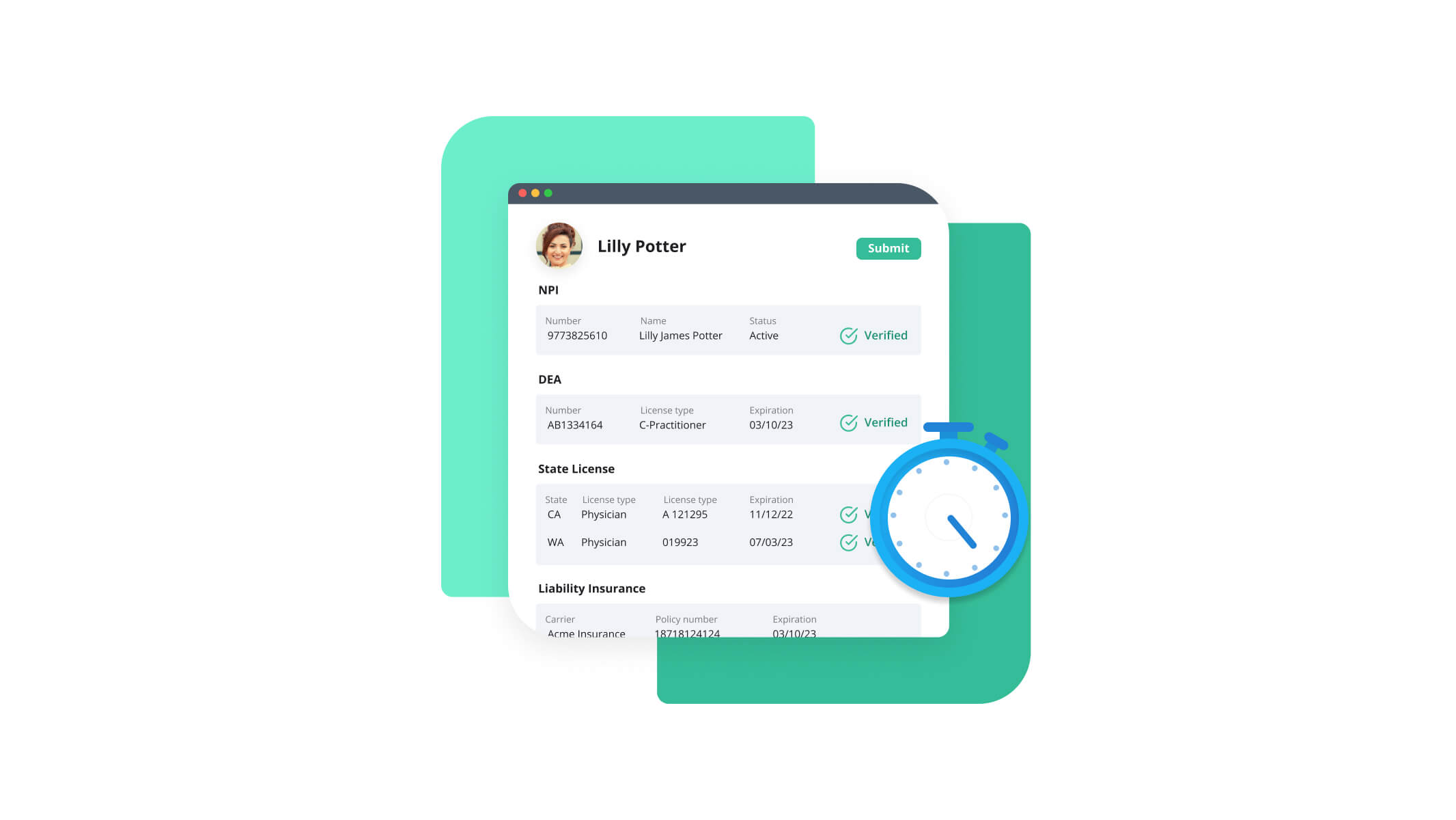
With Verifiable, your organization can directly access hundreds of primary sources to automate verifications in just seconds. Other benefits of this industry-leading compliance streamlining technology include:
- Real-time data: Verifiable has built technology directly to the various primary sources healthcare companies need most - supporting access to unparalleled data quality with information captured in real-time whenever you need it.
- Integration-friendly: Verifiable’s robust API integrates into the existing systems and workflows your organization uses most. Additionally, Verifiable’s technology can return validated, structured provider data that can be utilized for reporting and automated workflows.
- Automated AI logic: Verifiable’s data & APIs can help you streamline and automate manual processes and trigger required workflows to help your operations teams scale. Verifiable also applies smart-matching, taxonomy mappings and other rules logic to ensure that the results are the most accurate results possible
- Audit ready. Your organization and your data are always audit ready with timestamped audit logs and reports available.
- Path to Delegation. Verifiable has an experienced team of credentialing experts to help your organization formulate NCQA compliant policies & procedures, set-up your credentialing committee, and obtain delegated credentialing agreements.
Want to learn more? Dive deeper into learning about delegated credentialing in our complimentary handbook.
If you have questions or are looking for help in any of these critical areas - be sure to get in touch and we’ll be glad to help!