Verifiable is focused on rebuilding the infrastructure of trust for provider networks. Dooies's role involves leading the product and design teams in reimagining what credentialing can be in the future state by leveraging current tech.
Credentialing &
Monitoring That
Scales With You
Discover credentialing solutions designed to optimize provider networks, powered by industry-leading primary source verification technology.
.webp)


























Verifiable® Solutions
Whether your network is 100 providers, or 1 million, unlock immediate cost and time savings with pre-built credentialing solutions that centralize data, automate workstreams, and enable always-on compliance.
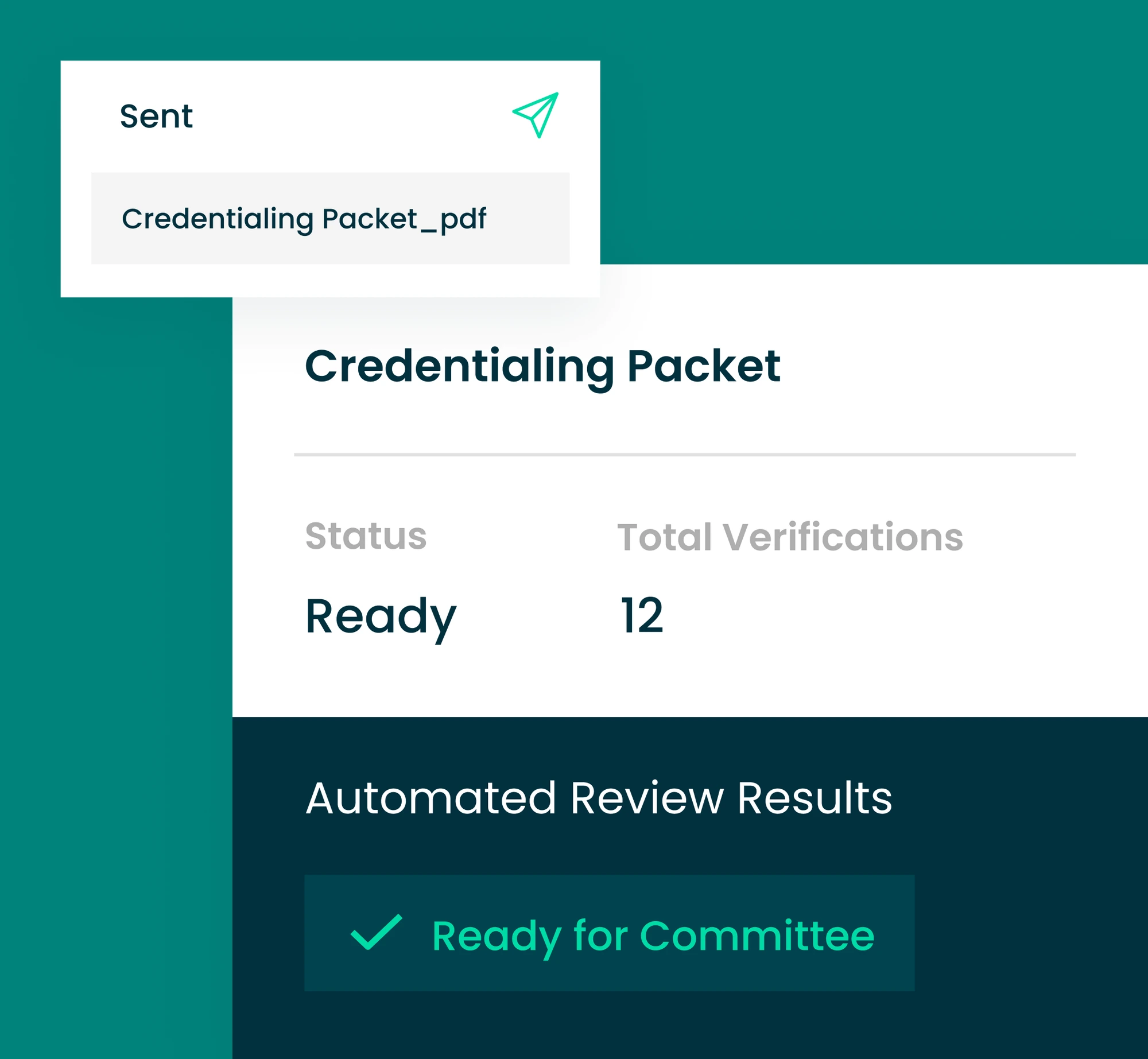
Error-Free, Fast Credentialing
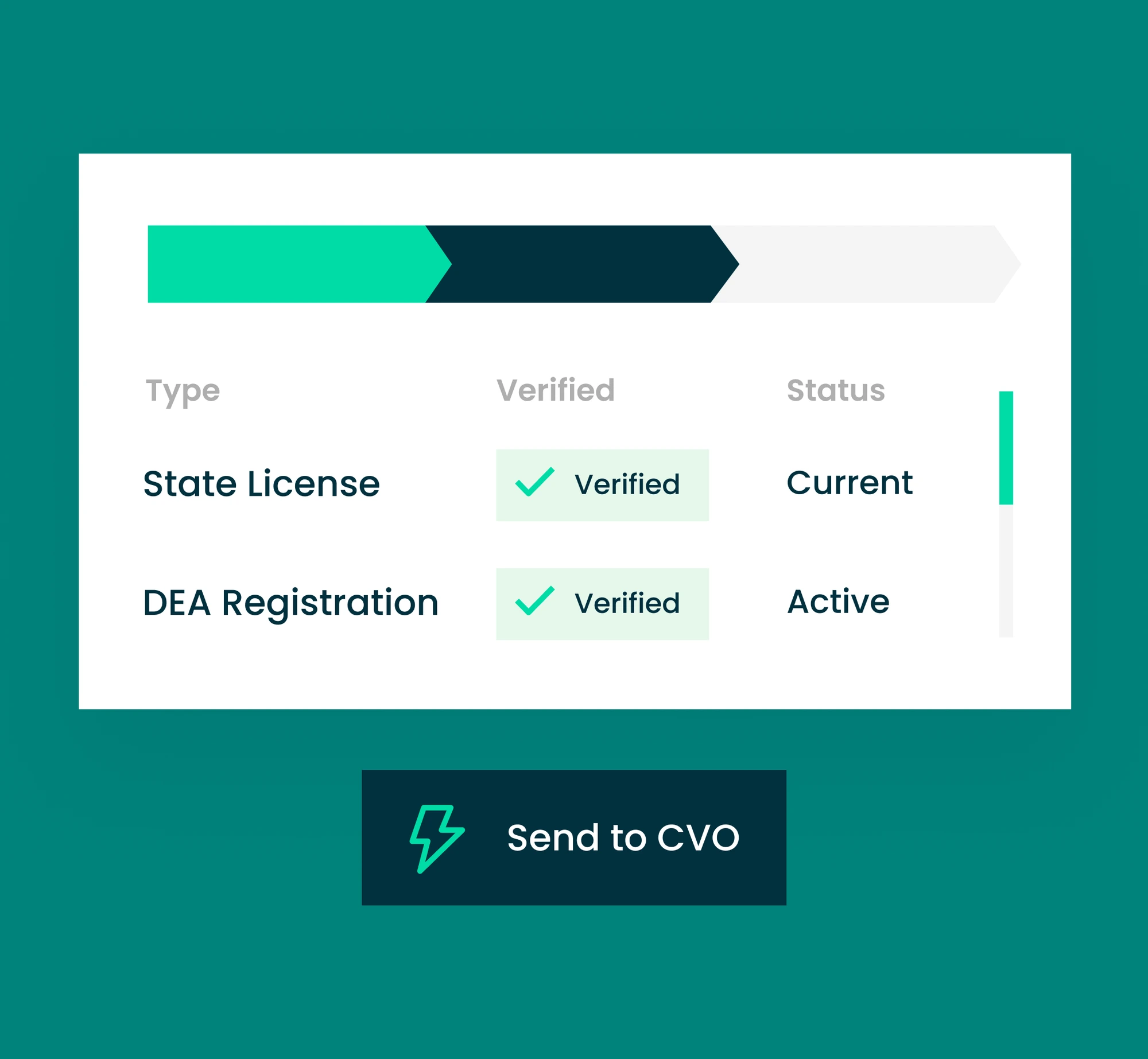
Proactive Network Monitoring
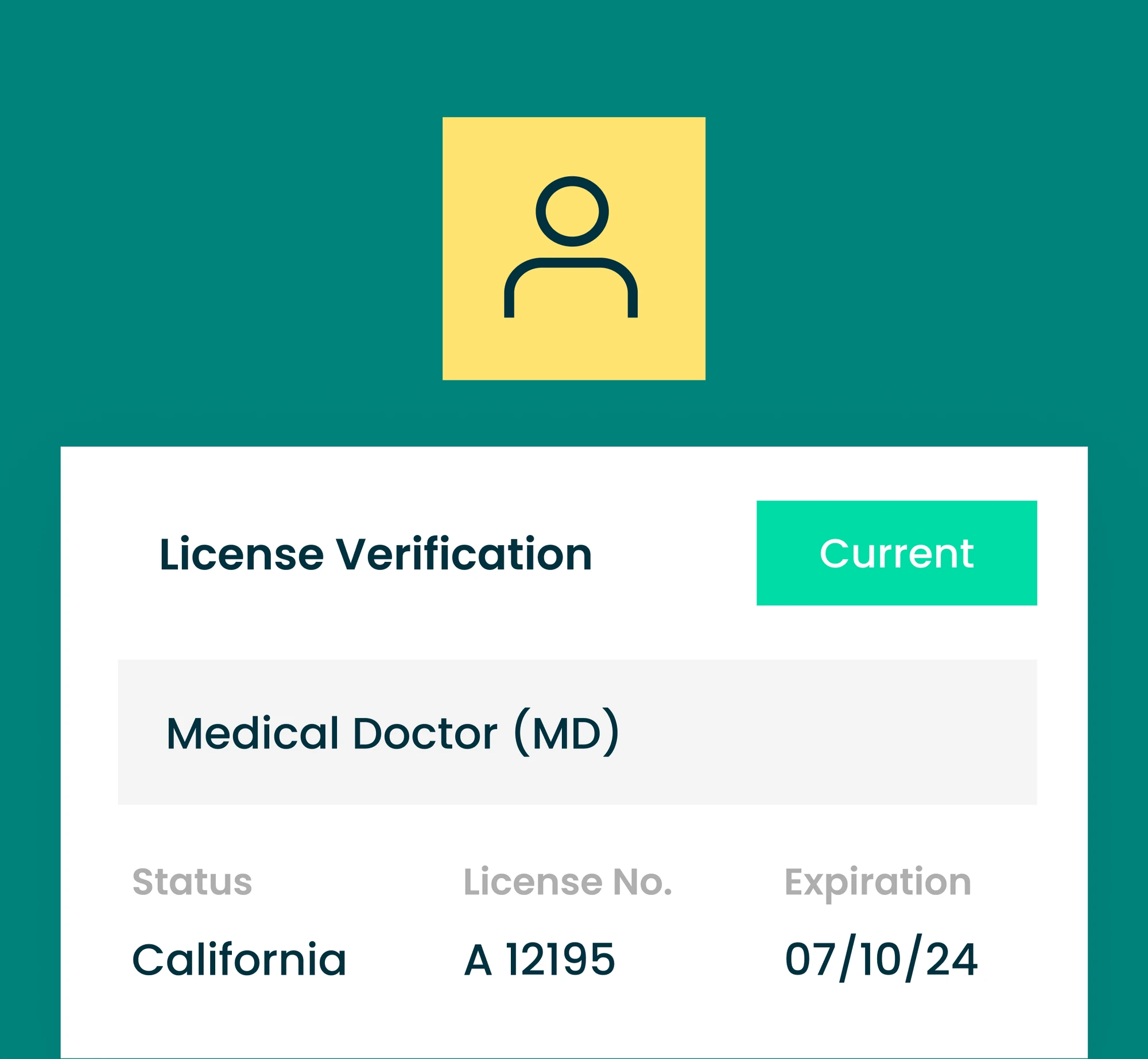
Real-Time Primary Source Verifications

COVERAGE
fully integrated verification sources
AUTOMATION
of verification results returned in seconds
SCALABILITY
verifications processed each month
Powering the Healthcare Ecosystem in Building Optimal Provider Networks
Health Plans
Optimize your provider network operations to strengthen compliance, save costs, and gain efficiency.
- Get providers in-network faster
- Save costs by bringing credentialing in-house
- Minimize risk in your provider network
- Gain control and visibility across your provider data
Provider Organizations
Eliminate the credentialing bottleneck and get providers seeing patients (and generating revenue) faster.
- Easier intake of provider information
- Capture missed revenue
- See credentialing status in real-time
- Appeal to payers when pursuing delegated contracts
Stories from our Customers
Being able to have that real-time access to credentialing status in Salesforce and having it be so easy to use and understand, is huge for us.
Holly Long
Director of Operations

Verifiable's Salesforce application was so easy to deploy. They'd really thought of everything! Beyond saving us a ton of development time & costs, Verifiable helped us reconcile and improve our provider data quality, which is invaluable.
Daniel Hoffman
Salesforce Administrator

Our consistent turnaround times combined with a robust focus on NCQA standards has become a top selling point when facilitating contracts with new payer partners.
Christy Maselli
Director of Strategic Operations








A Pre-Built Application for Seamless Credentialing and Network Monitoring on Salesforce
Discover the Power of Salesforce + Verifiable



.svg)
.png)