
The Future of AI Credentialing has Arrived
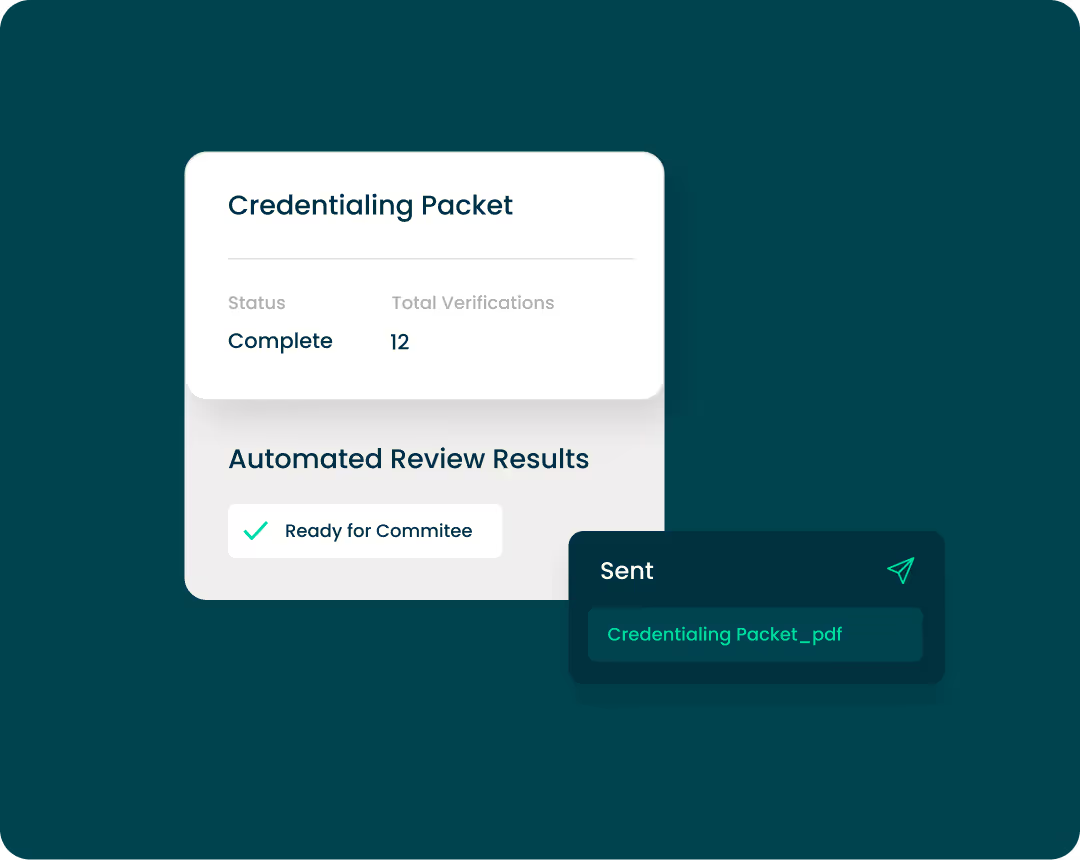
CredAgent™ is the first autonomous agent built to unlock 10x team productivity and improve operating margins, without sacrificing audit-ready accuracy.









Backlog to Batch Processing
Move beyond single-file workflows. Process thousands of credentialing events in parallel to handle seasonal spikes or network expansions instantly.
Fully Transparent AI
CredAgent provides step-by-step decision logs and cited primary sources for every verification. Your committee gets speed and full auditability.
Custom Governance
Configure the agent to follow your specific business rules and NCQA policies, ensuring every automated decision meets your unique risk standards.
Unlock a Scalable Model for Provider Credentialing
Expanding provider networks has traditionally meant expanding headcount proportionally, but Verifiable changes that. Whether your network is 100 providers, or 1 million, you can unlock immediate cost and time savings, out-of-the-box compliance, and enterprise-grade scalability with Verifiable’s credentialing and monitoring solutions.
7-figure Cost Savings
98% Increase
In Packet Turnaround Efficiency
100%
NCQA Scorecard & Audit Pass Rate
Verifiable Offers Unmatched Flexibility & Reliability in Credentialing Solutions
Multiply team efforts, centralize data,
and enable audit-ready compliance.
and enable audit-ready compliance.
Credentialing Automation Software
Automated PSV technology improves turnaround times and ensures compliance with real-time data, automated workflows, and self-serve insights designed to streamline your credentialing function.
Remove credentialing backlogs and data silos with:
- Simplified provider applications
- Primary source verifications in seconds
- Automated packets for committee review
Explore Credentialing Software
NCQA-Certified CVO
Backed by powerful automation and expertise, our CVO streamlines the entire process to meet NCQA and custom policies with greater efficiency
Have confidence in CVO-completed credentialing with:
- <3 day turnaround times
- 0% error rate for file quality review
- 100% NCQA audit pass rate
Explore CVO Services

Ongoing Provider Monitoring
Stay ahead of compliance risk with automated monitoring across key data sources and proactive provider license expiration alerts.
Meet or exceed NCQA standards with:
- Flexible monitoring frequency
- Self-serve reporting and insights
- Match review and intervention management
Explore Monitoring Software

Looking for additional provider data products and offerings like enrollment, licensing, roster management, and more?
What Do Customers Have to Say About Verifiable?
A Credentialing Platform That Scales to Millions of Providers Across the Healthcare Industry
Health & Dental Plans
Optimize your provider network operations to strengthen compliance, save costs, and gain efficiency.
Get providers in-network faster
Save costs by bringing credentialing in-house
Minimize risk in your provider network
Gain control and visibility across your provider data
Learn more
Provider Organizations
Eliminate the credentialing bottleneck and get providers seeing patients (and generating revenue) faster.
Get providers in-network faster
Save costs by bringing credentialing in-house
Minimize risk in your provider network
Gain control and visibility across your provider data
Learn more
Don’t see your organization type here?
Verifiable works with organizations across healthcare, including pharmacy, recruiting and staffing, and life sciences.
Learn more
Seamless Credentialing and Provider Network Monitoring on Salesforce
As a pre-built native Salesforce application, Verifiable helps you achieve proven faster time to value by extending the Salesforce platform with data
Discover the Power of Salesforce + Verifiable
Verifiable Leads the Way in Credentialing Innovation

AI Explained: The Intersection of System Safety, Generative AI, and Healthcare Credentialing with Brett Dooies
Read Story

Building a Smarter Future: How Our Credentialing Team is Leading the AI Revolution
Learn More


.svg)




