Automating provider roster imports without sacrificing accuracy or compliance
Verifiable is launching Roster Management for Health Plans on Salesforce, a solution that automates and standardizes provider roster imports while strengthening data accuracy and regulatory compliance.
Health plans receive provider rosters at volume every month. Each file represents the most up-to-date view of the network: enrollment status, practice locations, specialties, panel status, and contact information.
But processing even a single roster can take weeks.
Provider data imports remain largely manual. Operations teams reconcile spreadsheets, interpret inconsistent file formats, normalize data fields, and track changes line by line. With limited visibility into what actually changed from one submission to the next, updates move slowly, teams are stretched thin, and small errors can create outsized compliance risk.
Delegation and leased networks don’t eliminate that risk.
Under CMS, NCQA, and state regulations, health plans retain full accountability for timely directory updates, sanctions screening, and maintaining audit-ready documentation across their entire provider network.
As roster volume grows, so does operational strain and exposure.
How we streamline roster imports to eliminate network friction
Rather than adding another workflow layer on top of spreadsheets, Verifiable standardizes and governs roster data at the point of import so updates move faster without introducing compliance risk.
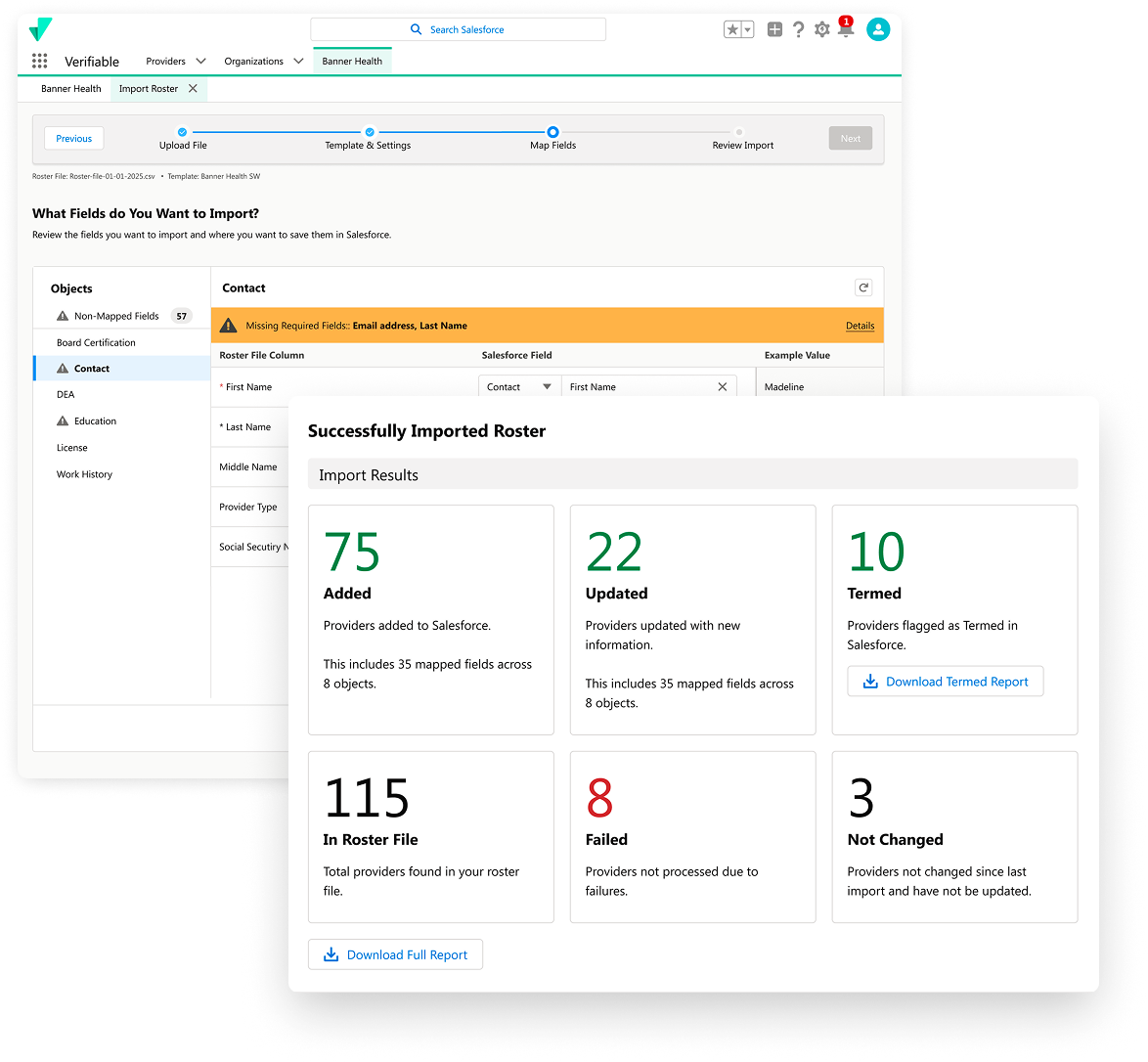
Configurable, reusable import templates
Map incoming roster formats once and reuse templates at scale. Flexible data mapping adapts to each partner’s file structure without requiring repeated manual rework.
Built-in governance and validation controls
Enforce validation rules, deduplication logic, and required-field enforcement ensure data is standardized and compliant before it enters your network.
Pre-submission impact visibility
Preview exactly how a roster will affect your network–including providers added, updated, or termed–before committing changes. No more blind imports.
Clear, actionable error reporting
Download detailed error reports that pinpoint failed records and the specific reasons behind them, enabling faster resolution and resubmission.
Integrated compliance monitoring
Automatically trigger sanctions and license monitoring on newly ingested providers, supporting ongoing adherence to CMS, NCQA, and state requirements.
Conclusion
Manual roster processing doesn’t scale. As network complexity grows and regulatory scrutiny intensifies, health plans need a faster, more governed way to ingest and manage provider data.
Verifiable’s roster management solution standardizes imports, enforces data governance, and provides the visibility teams need to move quickly without sacrificing compliance.
Ready to eliminate manual reconciliation and bring clarity to roster updates?
Get a demo of Verifiable Roster Management and see how it transforms provider data operations.

.svg)