Always-On Provider Network Monitoring Technology
Protect your organization with provider monitoring that flags issues before they impact your compliance. Monitor thousands of sources for sanctions, license expirations and more.


Verifiable’s Automated Provider Network Monitoring for NCQA Compliance and Beyond
Risk Mitigation
Stay compliant with continuous monitoring of NPDB, OIG, SAM, Medicare Opt-Out, State S&Es, and OFAC.
Cost Savings
Prevent revenue loss from denied claims due to lapsed licenses.
Scalability
Automate verification logic to confirm matches and remove false positives, so your team only reviews real risks.
We’ve Got You Covered
Driven by our robust primary source verifications, monitoring is available to organizations using our credentialing technology solutions, CVO services, or as a standalone solution.
Monitor 100+ provider types
Expansive coverage of sources automates PSVs for more than just physicians
Capture board actions
From disparate sources outside of license verification
Disciplinary action documentation
Save documents attached to a provider’s license
Screenshots for NCQA standards
Adhere to compliance guidelines
The Provider Network Monitoring Features that put Compliance on Auto-Pilot
Don’t wait for a compliance breach to take action. Designed for automation and transparency, we automatically activate monitoring for all providers across key data sources to meet and exceed NCQA standards.
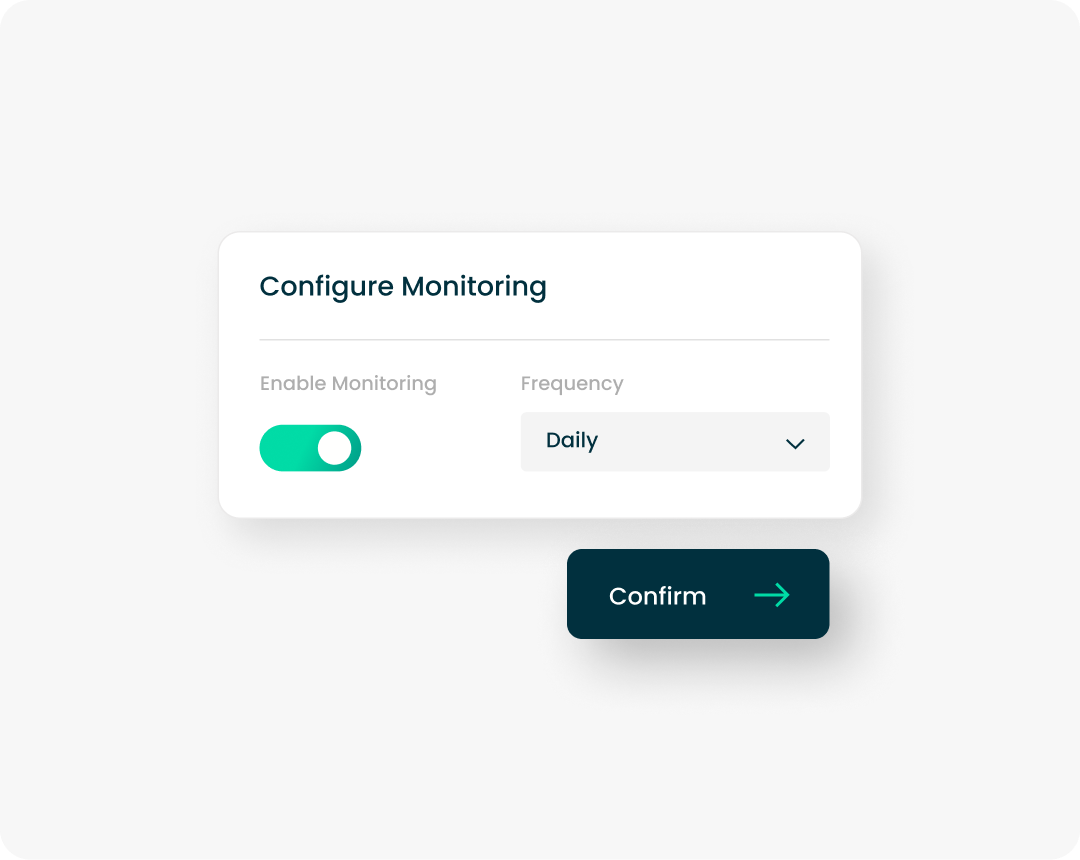
Automated Monitoring Enrollment
Manual verifications are not keeping up with monitoring requirements. Consolidate NCQA-compliant primary sources to simplify checks & receive provider updates in real time.
Proactive Provider Expiration Notifications
Eliminate the manual chase. Automatically notify providers of upcoming credential expirations with clear instructions to keep them in good standing, preventing operational setbacks before they happen.
Integrated Match Review & Intervention
Centralize your investigation workflow. Enable termination actions, sanction exclusion approvals, and deep-dive investigations directly within the platform to suppress false alarms or address hits immediately.
Self-Serve Reporting & Insights
Be audit-ready every day. Access pre-built, configurable dashboards that provide real-time views into the health of your network, ensuring you never miss a detail during regulatory checks.
Platform Delivery: Built for Your Tech Stack
Whether you need a standalone solution or a deep integration, Verifiable fits seamlessly into your existing IT infrastructure to support scalability and interoperability.
Native Salesforce App
Leverage the "Verify and Monitor" package directly within your Salesforce environment for automated license monitoring without leaving your CRM.

Learn more about the Salesforce Experience
Flexible API Integration
Connect our monitoring engine directly to your existing systems to automate data exchange and support custom workflows.
Standalone Web Application
Access powerful monitoring tools immediately through our secure, cloud-based web portal—no complex implementation required.
Out-of-the-Box NCQA Compliance Made Easy with Verifiable
Organizations relying on more traditional, typically manual methods for network monitoring may struggle to keep pace with NCQA-recommended monitoring frequency. Explore the chart below and see how Verifiable’s more frequent monitoring can help your organization stay ahead of all NCQA requirements.
Source | Purpose | Required | NCQA monitoring frequency |
|---|---|---|---|
NPDB | Continuous query for real-time notifications of adverse actions taken against providers. | Yes | Daily |
Sanctions & Exclusions: State | Checks compliance with state regulations by excluding providers disciplined by state enforcement agencies. | Yes | Monthly |
Sanctions & Exclusions: OIG | Verifies that providers are not excluded from federal reimbursement programs due to misconduct or fraud. | Yes | Monthly |
Sanctions & Exclusions: SAM | Screens for debarred or excluded individuals or entities to prevent potential fraud. | Yes | Monthly |
Medicare Opt-Out | Identifies providers who choose not to receive reimbursement from Medicare to avoid billing issues. | Yes | NPDB |
NPI | Simplifies financial transactions to review a provider’s NPI for verification and avoid unexpected billing delays (a HIPAA initiative). | Recommended | Monthly |
State Licenses | Verifies healthcare providers’ educational background, professional qualifications, and passing of necessary examinations so they can practice legally with their state. | Recommended | Monthly |
DEA | Simplifies financial transactions to review a provider’s NPI for verification and avoid unexpected billing delays (a HIPAA initiative). | Recommended | Monthly |
SSA-DMF | Checks against deceased persons to prevent fraudulent activity. | Recommended | Monthly |
OFAC | Ensures providers and partners are not associated with sanctioned or restricted entities. | Recommended | Monthly |
CMS Preclusion | Identifies healthcare providers and prescribers who are precluded from receiving payment for Medicare Advantage (MA) items and services, as well as Medicare Part D drugs. | Recommended | Monthly |

.svg)

